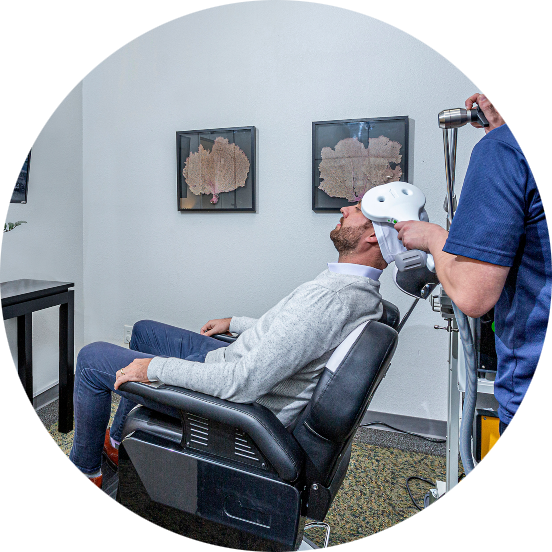
TMS (Transcranial Magnetic Therapy) has been F.D.A. approved, since 2008 – yet so many veterans and even many clinicians do not know about the scientifically proven, hugely effective outcomes TMS provides for numerous psychological illnesses, as well as physiological issues.
When TMS is provided in conjunction with concentrated individual and group therapy, it actually cures, or massively reduces the symptoms of depression, anxiety, trauma, suicidal thinking, ADHD, OCD and so many other mental disorders.
Individuals who have never obtained healing from their illness(s) through other treatments are finally able to heal through TMS.
Our scientific assessment data, collected on hundreds of patients, convincingly proves how life-changing TMS + psychotherapy are in healing veterans.
Please refer to our TMS page for additional information.